Paola passed away with dignity and respect, on her terms, thanks to her honest and direct conversations with her family…and a POLST form. She always said, she trusted that God knew when it was her time, and she did not want any artificial life extending measures. She did not want to live as a vegetable or severely disabled. She only wanted to live if she could be Paola and do all the things Paola loved to do. Despite being 85 years old, fiercely independent, and with a history of falls, she and her family only learned about POLST forms three months before her passing thanks to a serious fall on April 24, 2023. After that fall, Paola made sure her family understood her end-of-life wishes almost daily and made sure to put it in writing.
What are often termed “heroic” life saving medical procedures are often futile, and unnecessarily prolong the suffering for the patient and their family. What is also not widely known is that resuscitation measures are violent, particularly for the elderly. Senior patients often suffer broken ribs or sternum, internal bleeding or collapsed lungs from CPR chest compressions. Some get pneumonia from stomach fluids entering the lungs. Intubation can causes irreversible damage to air pathways. And if they survive, many patients suffer serious neurological impairments from lack of oxygen to the brain. One published study in the The Journal of the American Geriatrics Society found that only 19% of patients 80 years or older return home after having been intubated. Yes, there are ways to keep patients technically alive for weeks or months, but what is the quality of life for them (and their families) in their final days?
Read more about this topic in this May 2023, Atlantic Magazine article written by an ICU nurse.


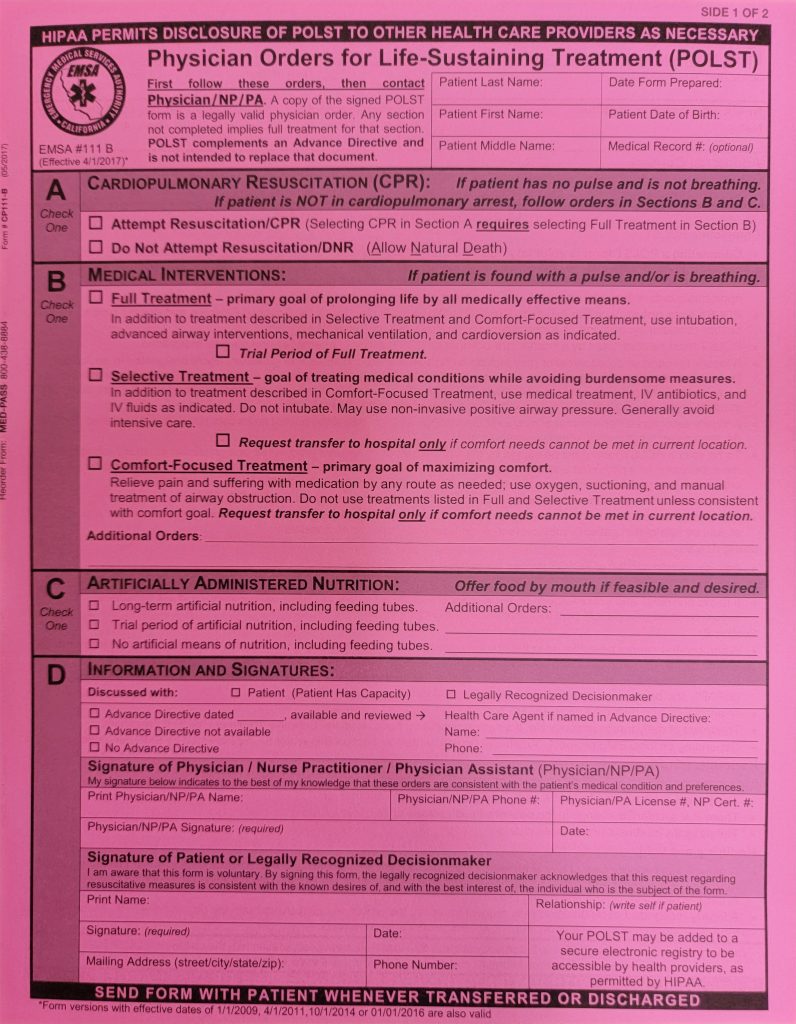
What is a POLST Form?
POLST stands for Physician Orders for Life Saving Treatment. If you or your loved ones are elderly, frail or have chronic health issues, this form tells medical personnel what type of treatment you give permission for them to administer in the event you are not conscious or able to speak for yourself. If you want medical personnel to keep keep you alive at all costs, then you probably don’t need a form. That is the defacto treatement by emergency responders and physicians. If you or your loved one do not want to be resuscitated, intubated or given artificial food through tubes for prolonged periods of time, then you need a form so your family and the doctors can respect your end of life wishes. In a moment of trauma, with only seconds or minutes to act, the POLST form is essential.
Read more about POLST forms, sample conversations, myths & facts and more on the UCLA Health website.
What to do with a POLST Form
Make sure to complete and use the form correctly to respect your loved ones end of life wishes.
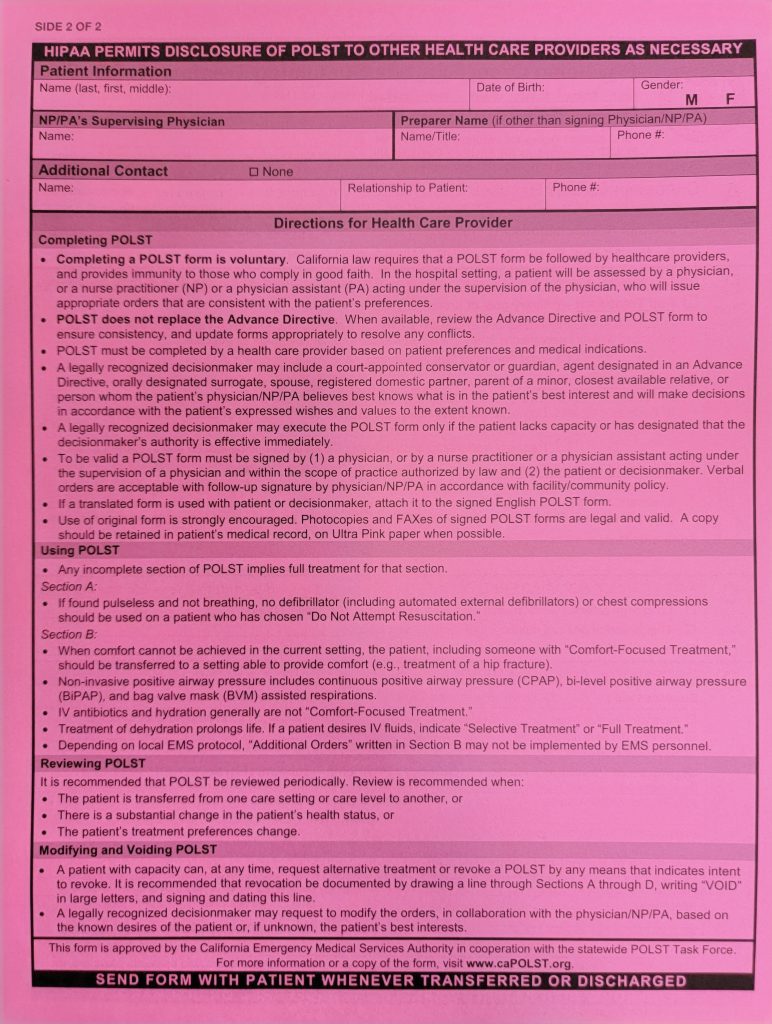
- Get the Form: Ask your or your loved one’s primary care physician for at least two POLST forms or print POLST Forms HERE (on bright pink paper). Find multilingual POLST forms HERE. If you live in the Bay Area, you can also reach out to Eduardo and pick up blank forms from him.
- Have the Talk: Have the conversation with loved ones about their end of life wishes.
- Sign it: Make sure you or your loved one AND their physician signs it. (Paola’s form only had her signature, which caused difficulties honoring her wishes at the hospital).
- Keep it Handy: For vulnerable loved ones, especially for those living alone, keep a copy of the POLST form on the refrigerator or on the night stand. Emergency medical personal will only look for a split second in easy-to-see places before providing treatement. Keep another copy in your car as well, in case a medical emergency happens suddenly and your loved one is transported to a different hospital. (Eduardo thankfully stopped at home to retrieve Paola’s POLST form, before heading to the hospital).
What a POLST Form looks like: